
Nail psoriasis is a specific form of psoriasis that affects the nails on the hands and / or feet. Doctors call this type of disease psoriatic onychodystrophy (Greek).onychos- nail,dys- violation,cup- food).
In this article you will learn the causes of the development of nail psoriasis, the symptoms that do not always show a correct diagnosis, and dangerous misconceptions about this form of the disease.
Note.There are many photos in the article that can scare an unprepared reader.
Where do nails grow?
To understand the problem of nail psoriasis, it is important to understand how the so-called nail apparatus works.
The nail has two functions: functional and aesthetic. First, the nail protects the fingertips from damage, increases accuracy and sensitivity when working with small objects, can be an offensive or defensive weapon, and finally, we itch with the help of nails. Second, the aesthetic or cosmetic function of the nails is also important, especially for women.
Nails are formed from the outer layer of the skin - the epidermis. The nail apparatus includes:
- nail plate - directly on the nail itself,
- matrix - produces nail plate,
- The nail hole, or lunula, is the only visible part of the matrix, it is a place in the shape of a white moon at the base of the nail plate,
- eponychium - a nail roller that protects the matrix from damage from above,
- nail bed - is located under the nail plate and is responsible for attaching the finger to the nail phalanx,
- hyponychium - the transition zone between the nail bed and the skin of the fingertip.
Causes and mechanism of development of nail psoriasis
In the course - with periodic exacerbations and remissions - psoriasis on the nails resembles a vulgar form of the disease.
It is believed that nail psoriasis develops for the same reasons and in the same way as typical psoriasis eruptions. There are external and internal factors among these reasons.
The main internal factor is genetic predisposition. There are many external causes, such as injuries, poor diet, intoxicants (alcohol and tobacco), infections, and some medications.
The standard mechanism of development of nail psoriasis under the influence of these causes can be briefly described as follows:
- Triggers such as trauma activate immune cells.
- Activated immune cells migrate to the area of the nail matrix or nail bed.
- Immune inflammation develops in these areas.
- The division of skin cells is accelerated and their maturation is disrupted.
- Nails have characteristic psoriasis symptoms.
In addition, the cause of nail psoriasis can be attributed to the body's inability to adapt to adverse environmental conditions. In this sense, the main cause of psoriasis is an evolutionary foreign environment.
As a result, this evolutionary approach considers harmful nutrition, lack of sun and clean water, excess toxins, lack of normal physical activity, sleep disorders and chronic stress as the direct causes of the disease.
Nail psoriasis and psoriatic arthritis are related
The link between nail injury and psoriatic arthritis has long been known.
According to observations, scientists have found that psoriatic arthritis is accompanied by nail damage in nine out of ten cases.
However, the mechanism of this connection has not been fully studied. However, the authors of a number of studies, such as the Institute for Molecular Medicine in Leeds (UK), have tried to explain this connection beyond the concept of immune inflammation.
According to them, the finger joint is located near the nail and is anatomically connected with it.
Therefore, the Kebner phenomenon, which causes microtrauma and primary joint inflammation - psoriatic arthritis - also causes secondary pathological changes in the nearest nail.
This is why psoriatic arthritis is often associated with nail damage.

Thus, the symptoms of nail psoriasis are often an indication of psoriatic arthritis.
Now let's look at the main myths that accompany this disease and how dangerous they are.
Myth 1: Nail psoriasis is rare.
In fact, no. As you can see, nails with psoriasis suffer very often.
According to various sources, nail psoriasis accounts for 6% to 82% of cases of psoriasis vulgaris. Such a wide prevalence in the assessment of the prevalence of this pathology is explained by problems with its accounting. Medical statistics show that patients with a vulgar form first seek medical attention, and secondly, attention is paid to the nails. In scientific research, cases of nail psoriasis are generally studied only in addition to the main object of interest - psoriasis with skin lesions.
But a number of publications say so
Recurrent nail damage has been reported in up to 80-90% of patients with psoriasis vulgaris.
Also, psoriasis of the nails occurs in 90% of patients with psoriatic arthritis and psoriasis of the scalp.
It should be noted that in general, adults suffer from this form of the disease.
According to various sources, nails in children are affected in about 7-37% of cases of psoriasis. Unfortunately, the manifestations of psoriasis on the nails of a child are often not given due attention. Parents or doctors believe that this is the norm or a result of trauma, or they do not notice it because the symptoms are mild.
Myth 2: Nail psoriasis is easy to recognize by its symptoms
In fact, not always. That is a fact
The nail can respond to various diseases only with a limited number of symptoms. Therefore, the manifestations of different diseases on the nails may look the same.
Of course, if the patient has symptoms of severe psoriasis vulgaris, nail psoriasis can be suspected. However, nail lesions can be small compared to skin lesions and can be easily ignored by a doctor.
Usually, the more active psoriasis is on the skin, the more damage it does to the nails.
First of all, nails are affected.
It is also important to know that in 5% of cases, the nails may be the first manifestation of psoriasis. That is, the classic manifestations of psoriasis on the skin may be completely absent.
What a nail psoriasis looks like depends on where the pathological changes come from - the matrix or the nail bed.
The source of the symptoms - the matrix or the bed - should be considered when choosing treatment. Therefore, it must be defined correctly.
Symptoms of the nail matrix:
- high fever symptom,
- white spots and spots (leukonychia),
- red dots in the hole,
- broken nails.
Although the cause of these symptoms is at the matrix level, pathological changes occur in the nail plate as the nail grows.
The cause is the symptoms in the nail bed:
- nail bundle (onycholysis),
- longitudinal bleeding,
- subungual hyperkeratosis,
- symptom of oil stain.
Then we will focus on each symptom separately. And let's start with the manifestations of the matrix.
High symptom
The symptom of the nail is visible on the surface of the nail plate with holes or holes resembling sediments in the nail.
Such defects occur mainly in the nails, but rarely appear on the feet. As the nail grows, the holes move from the nail layer to the edge of the nail plate.
The holes in the nail psoriasis are usually deep, large and chaotic. It is caused by the accumulation of empty cells on the surface of the nail, which are damaged by keratinization.

The more severe the psoriasis, the more common the symptoms of tremor.
However, in addition to psoriasis, we must not forget that the holes in the nail are also characteristic of alopecia areata (alopecia), eczema, dermatitis, and can occur, for example, with a fungal infection.
Counting the number of holes in all the nails will help to make a correct diagnosis.
- Less than 20 - not typical for psoriasis,
- Between 20 and 60 - psoriasis may be suspected,
- Over 60 - Confirm psoriasis diagnosis.
White spots (leykonychia)
Leukemia is a symptom that manifests itself as white spots or spots on the nails.

With leukonics (from the Greek).leukos- white andonychos- nail), in contrast to the superficial pits in the symptom of high, the cells with impaired division and keratinization are located in the thickness of the nail plate. At the same time, the surface of the nail remains smooth. The white color of the spots is caused by the reflection of light from groups of cells placed in an empty space.
However, some studies have shown that leukemia is so common in healthy people that it is not a significant symptom of psoriasis. For example, damage to a manicure can cause leukonia.
The nails fall out
When superficial pits (high symptom) and deep leukonic zones (white spots) combine, the nails begin to fall out.

Typically, nail splitting occurs with long-term nail psoriasis.
And the more intense the inflammation of the nail matrix, the more the nail plate is destroyed. In severe cases, the nail can completely collapse and fall out.
Red dots on the nail socket
As you can see, red spots and general redness in the area of the hole are caused by increased blood flow to the veins under the nail.
In addition, the red dots in the hole are caused by a violation of the structure of the nail plate itself: it becomes more transparent and delicate. And for this reason, firstly the veins look better and secondly, the thin nail plate puts less pressure on the veins and is filled with more blood.

Thinning of the nail plate can also cause redness of the entire nail bed.
Nail shedding (onycholysis)
Now let's look at the symptoms, the source of which is the nail bed.
Onycholysis is the separation of the nail plate from the bed due to the accumulation of cells under the nail with damaged division and keratinization.

Onycholysis itself (from the Greek).onychos- nail andςις- separation) is not necessarily a sign of psoriasis and can develop, for example, as a result of nail injury.
Initially, the loss of contact between the nail and the bed occurs in the zone of hyponxia - along the outer edge of the nail plate. The onycholysis then spreads to the nail layer in a semicircular line. Due to the accumulation of air under the nail, the abrasion area turns white.
A reddish border (scientifically erythema) usually visible on the fingers at the edge of onycholysis is characteristic of psoriasis and helps to make a correct diagnosis.

With prolonged onycholysis, the nail bed loses its properties and the growing new nail is unlikely to adhere normally. Therefore, even with complete renewal of the nail plate, onycholysis often persists.
Onycholysis facilitates the penetration of bacteria and fungi, which can lead to infection. This sometimes causes the nail to change color. For example, when bacteria bind, a greenish color may appearPseudomonas aeruginosa(Pseudomonas aeruginosa) and others.
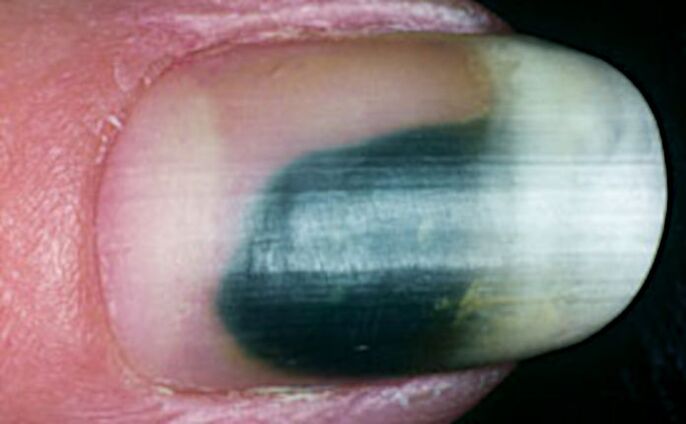
Longitudinal subungual hemorrhage
Longitudinal subungual hemorrhages occur in the nail bed and appear as a dark red line 1-3 mm long.
Increased blood flow and edema in the area of inflammation of the nail bed causes the rupture of capillaries, which manifests itself in the form of such bleeding.

Due to the nature of the blood supply, most bleeding occurs on the free edge of the nail - in the zone of hyponxia.
Subungual hyperkeratosis
Subungual hyperkeratosis is the accumulation of dead cells under the outer part of the nail plate.

Psoriasis, subungual hyperkeratosis (from the Greek).hyper- excessive andkeras- horn) is usually silver-white, but can also be yellow. When the infection is added, it can be, for example, green or brown.
The more the nail is removed from the nail bed, the higher the activity of the pathological process.
Subungual hyperkeratosis in the fingers usually manifests itself with loose layers under the nail plate. In the legs, these masses are tightly soldered with a thickened nail.

In addition, psoriasis, which is a lesion of the nails, is characterized by a combination of subungual hyperkeratosis with onycholysis (separation of the nail).
Fat stain symptom
Symptoms of oil stains appear in yellow-red (goldfish) spots under the nail plate.
They approach the nail bed in the nail bed and move towards the edge of the nail as they grow.

The cause of this symptom is inflammation of the nail bed with dilation of the capillaries and impaired accumulation and division and keratinization of cells involved in inflammation.
Oil stains come in different shapes and sizes. It can be found both in the center and on the edge of the nail, near the onycholysis zone.
Myth 3: Nail psoriasis is just a cosmetic problem.
In fact, this is not true. Although more than 90% of patients report having unpleasant psoriasis nails, this is not just a cosmetic issue.
According to various studies, nail psoriasis significantly reduces the quality of life of patients:
- 52% of patients also complain of pain,
- 59% - due to problems in daily activities,
- 56% - for difficulties at home and
- 48% - due to difficulties at work.

Therefore, it is very important to make a correct diagnosis and start treatment as early as possible, because improving the condition of the nails significantly improves the quality of life of patients with psoriasis.
Myth 4: Nail psoriasis is not dangerous
In fact, this is not the case. We have already written about the causes of this form of the disease
Nail psoriasis is an important symptom of psoriatic arthritis.
It is important to remember that the external manifestations of arthritis may not be complete. In this case, we can talk not only about the impact on the fingers and toes, but also about the joints of the spine and pelvis.
For arthritis, you can examine your joints with ultrasound (ultrasound) or magnetic resonance imaging (MRI).

Although there are no obvious symptoms of arthritis, but there are manifestations of nail psoriasis, it is very important to make sure that all joints are in order.
And then regularly monitor the condition of the joints. Otherwise, psoriatic arthritis can be easily missed! Late diagnosis will lead to late treatment and eventually irreversible joint damage and disability.
Therefore, if your doctor has not ordered an insurance study on the grounds that there are no visible signs of arthritis, you should go to the clinic yourself and, for example, undergo a paid ultrasound examination.
How to diagnose nail psoriasis
It is important to recognize that many of the symptoms of nail psoriasis described above can help make a correct diagnosis. However, nail changes that are characteristic of psoriasis can occur in other diseases, so it can be difficult to diagnose immediately.

In this case, the presence of several symptoms at the same time in different nails can help in the diagnosis.
The most important signs of psoriasis on the nails are:
- Symptoms of tremors: More than 20 holes in all nails of the hands indicate the possibility of psoriasis, and more than 60 holes confirm the diagnosis of psoriasis,
- Separation of the nail (onycholysis) with a reddish border on the edge,
- grease (salmon) stains on the nail bed.
Difficulties in identifying nail psoriasis with a single symptom
It is difficult to diagnose psoriasis if you have only one symptom.
For example, if onycholysis occurs only in the hands or subungual hyperkeratosis only in the arms and / or legs.
Probably the only method for a reliable diagnosis of isolated onycholysis (nail detachment) is the study of hyponhyroidism using a special microscope - dermatoscope.
A high-magnification video dermatoscope is used for this. Please note that the hand dermatoscope does not provide the required growth. All you need is a video dermatoscope magnified at least 40 times. Then enlarged capillary loops, which are characteristic of psoriasis, appear.

With isolated subungual hyperkeratosis, psoriasis is more likely to occur if the scales under the nail are whitish-silver, as well as if all the nails on the hands or feet are affected.
Pearl or nail fungus?
About 30% of patients with nail psoriasis also have a fungal infection - scientifically onychomycosis.
Externally, hyperkeratosis and onycholysis (separation of the nail) in psoriasis are similar to the manifestations of fungal infection. Therefore, it can be difficult to make a differential diagnosis, ie to determine the true cause of changes in the nail plate.
In addition, both psoriasis and fungus can affect the same nails at the same time. It often occurs in the toes and is primarily characteristic of elderly patients.
Also, with a fungal infection, one or both nails on the toes are often affected. In psoriasis, as a rule, several nails are affected at the same time.

The following symptoms speak in favor of psoriasis:
- oil stains and / or symptoms of tremors in your nails,
- signs of psoriasis on the scalp and / or large wrinkles on the skin,
- periodic remission and exacerbation of nail damage.
They say in favor of onychomycosis:
- longitudinal stripes on the affected nail,
- Detection of fungi on an affected nail under examination under a shaving microscope treated with potassium hydroxide (KOH test),
- positive culture for fungi.
In general, based on external manifestations alone, it is not possible to completely rule out fungal infection of the nails in patients with psoriasis.
We must not forget that a fungal infection can cause the Kebner phenomenon on the nail and surrounding skin, and this can result in psoriasis symptoms. Anyway
It is useful to consult a mycologist and do a test for fungi and start antifungal therapy if found.
Important findings and what to do
Let's summarize important information about nail psoriasis and its symptoms.
Diagnostic features:
- Nail psoriasis is very common, but is often missed.
- Manifestations of nail psoriasis can be small, so experts often do not pay attention to it.
- In 5% of cases, nail damage may be the only symptom of primary psoriasis.
- The manifestations of different diseases on the nails may look the same, which complicates the diagnosis.
The main manifestations of nail psoriasis:
- sign of high - holes in the nail,
- white dots,
- broken nails
- red dots in the area of the hole,
- nail set,
- longitudinal subungual bleeding,
- subungual hyperkeratosis - loose groups under the nail,
- symptom of oil stain.
Psoriasis and fungus:
- Psoriasis of the nail is often accompanied by a fungal infection.
- To rule out an unequivocal exception, it is necessary to contact a mycologist and conduct additional research.
Nail psoriasis and psoriatic arthritis:
- Nail psoriasis is a common companion of psoriatic arthritis.
- It is important to start treatment on time and detect pathological changes in the joints as soon as possible to prevent irreversible complications and disability.
- Although there are no symptoms of external arthritis and nail psoriasis is detected, the joints should be examined using ultrasound or MRI.























